Robotic single-site surgery versus laparo-endoscopic single-site surgery in ovarian cystectomy: A retrospective analysis in single institution
Article information
Abstract
Objective
Robotic single-site (RSS) surgery is being utilized in gynecologic surgery. However, its cost-effectiveness and limitations of the system make the application of the technique to benign surgery controversial. We compared the surgical outcome and learning curve of RSS to those of laparoendoscopic single-site (LESS) surgery.
Methods
Patients who underwent ovarian cystectomy from January 2013 to December 2018 at Korea University Anam Hostital were divided into two groups according to the surgery: RSS or LESS. After exclusion of ineligible patients, 29 patients who underwent RSS surgery and 80 patients who underwent LESS surgery were included in this study. Surgical outcome data regarding bleeding, surgical time, length of stay, and the learning curves of surgical time were obtained using the cumulative sum method.
Results
Patient demographics showed no differences between the groups except for tumor histology. There were no differences in bleeding, postoperative length of stay, surgical wound complication, or surgical preparation time between the groups. RSS surgery had a longer surgical time than LESS surgery (130.41 vs. 96.96 minutes; p<0.001). In a learning curve analysis, seven cases were required to be proficient in docking the RSS system. Comparing the learning curves of surgical time, RSS surgery required fewer cases to attain proficiency than LESS surgery (19 vs. 22 cases).
Conclusion
RSS ovarian cystectomy is a feasible and safe option with the benefit of a quick learning curve. The longer surgical time could be overcome with further improvement of surgical techniques and development of the robotic instruments.
INTRODUCTION
Laparoendoscopic single-site (LESS) surgery has been introduced into the field of gynecologic surgery, which has the benefit of minimal scarring [1-3]. Beyond overcoming surgical limitations in angulation and device manipulation, this technique has been applied even in surgeries with a high degree of difficulty [4]. However, surgeons need a prolonged learning curve period to achieve a proficiency without technical difficulties. Among diverse laparoendoscopic surgical techniques, intracorporeal suturing of ovarian tissue after ovarian cystectomy is one of the most difficult procedures and it is difficult to become skilled at the technique in a short period.
The robotic surgical technology has improved visualization and surgical dexterity, and surgeons can try the surgical techniques of laparotomy in minimally invasive surgery due to the ergonomic layout. Though robotic single-site (RSS) surgery may not be utilized as much as multiport robotic surgery, it still has benefits in terms of intracorporeal suturing, avoiding crush by surgical instruments, and the materialization of triangulation compared to LESS surgery [5]. Further, patients with benign ovarian tumors including mature cystic teratoma, cystadenoma, or endometriosis, are usually in childbearing age, and they may be sensitive and have anxiety regarding surgical scars [6]. Additionally, suturing remnant ovarian capsule provides the benefit of avoiding thermal damage to ovarian tissue in preserving ovarian function. The aims of this study were to compare surgical outcomes of LESS and RSS surgeries for adnexal tumors and to investigate if RSS surgery is feasible for a patient with a benign adnexal mass.
MATERIALS AND METHODS
1. Patients
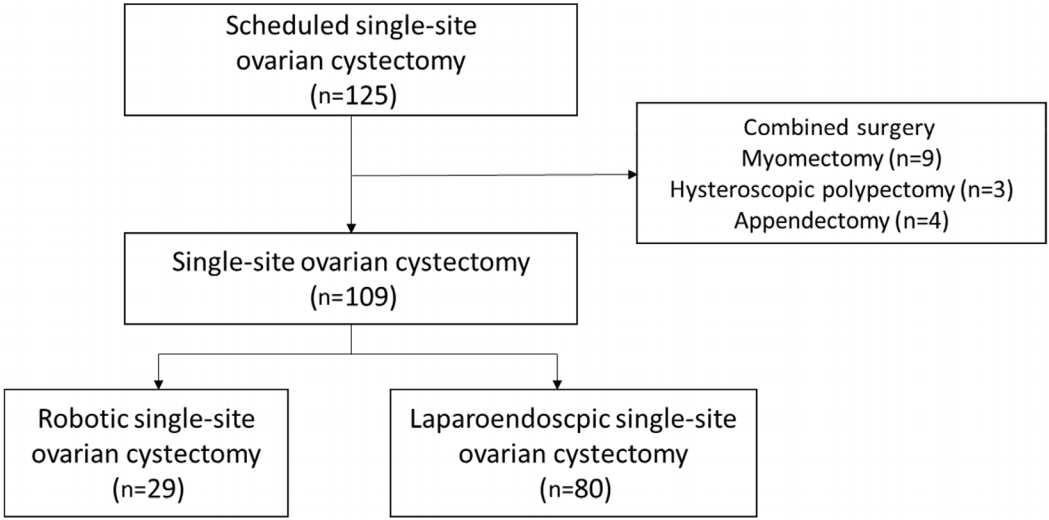
This retrospective study evaluated 125 patients with benign ovarian tumor lesions who underwent ovarian cystectomy using either LESS or RSS in our institution (Fig. 1). There were 16 ineligible patients because of the use of an additional port or a combined surgery. Finally, 29 patients underwent RSS and 80 patients underwent LESS from January 2013 to December 2018.
2. Surgical techniques
In LESS surgery, a 15–20 mm umbilical incision was made with the Hasson method. A Lapsingle® trocar (Sejong Medical, Co. Ltd., Seoul, Korea) or an Octo™ Port trocar (Dalim-SurgNET Co. Ltd., Seoul, Korea) was used for instrument application. Ovarian cystectomy was defined as a surgery peeling only the cystic tumor lesions and sparing all intact ovarian tissue and the uterus. The tumors were removed by cystectomy and the contralateral ovary was preserved. We used delayed absorbable suture devices in all patients for remnant ovarian suture by an intracorporeal continuous running suture method. All resected tumors were removed using a surgical bag to avoid tissue dissemination. After surgery, the umbilical incision was closed layer by layer from the fascia to the skin.
A da Vinci Si or Xi surgical system (Intuitive Surgical Inc., Sunnyvale, CA, USA) was used for RSS surgery. This included the same surgical procedures of LESS surgery, but only a Lapsingle® trocar was used for docking the robotic arms. A central arm for the laparoscope was inserted, and then the other two arms were located. During the surgery, the surgical procedures were not different from those of LESS surgery. All resected tumors were also removed using a surgical bag. At the end of the surgery, the umbilical incision was closed in the same manner as in the LESS procedure.
3. Statistical analysis
Variables such as patient age, body mass index (BMI), histological test results, operative time (preparation time and operating time), estimated blood loss, days of hospitalization, and complications were analyzed under the ethical board’s approval. Preparation time was defined as the time from applying anesthetic agents to incision time and surgical time was the time from first incision to the time of closure. Docking time was checked only in RSS surgery, and it was the time needed for the docking of the robotic devices.
Learning curves were analyzed by consecutive cases using the cumulative sum (CUSUM) method. A CUSUM analysis was used to quantitatively assess the learning curve of docking time and surgical time (CUSUM-DT and CUSUM-ST, respectively). This technique provides a graphical representation of the trend in the outcome of consecutive procedures performed over time since it is a plot of the cumulative total of differences between each data point and the mean of all data points. This approach gives a visual representation of the learning curve.
We used the IBM SPSS Statistics software (version 22.0; IBM Corp., Armonk, NY, USA) for the statistical analysis. A Kolmogorov-Smirnov test was used to verify the standard normal distribution assumptions. A Student’s t-test and a Mann-Whitney U test were used for parametric and nonparametric variables, respectively. Differences between proportions were compared using a Fisher’s exact test or a chi-squared test. A level of significance was established as P<0.05 for all statistical tests.
RESULTS
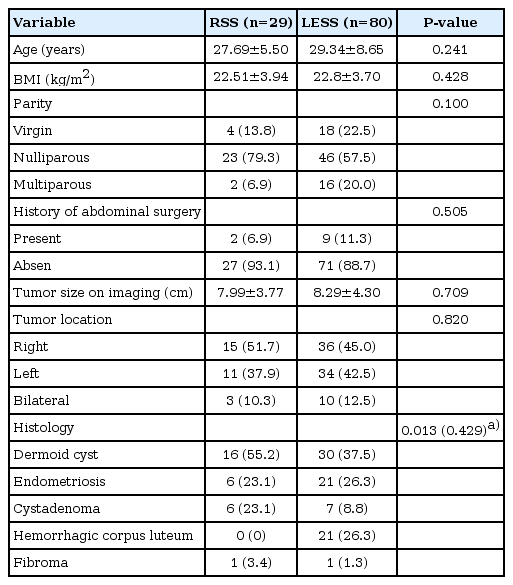
The patient demographics are shown in Table 1. No significant statistical differences were found with respect to age, BMI, parity, history of abdominal surgery, tumor location, and suspected tumor size on imaging including ultrasonography, computed tomography, or magnetic resonance imaging. However, tumor histology was different between the two groups because of the inclusion of emergency surgery of the hemoperitoneum due to rupture of the hemorrhagic corpus luteum or a torsion of a dermoid cyst. This difference was resolved after the exclusion of these cases.
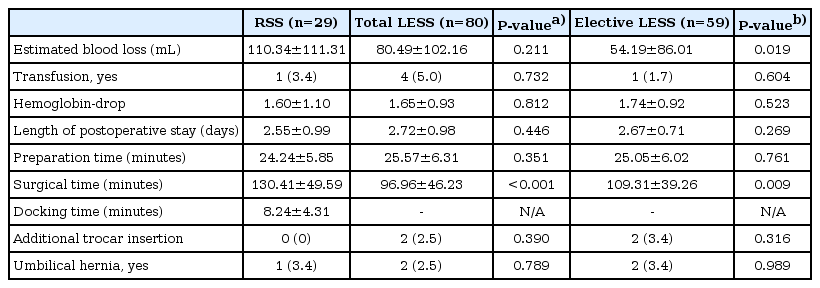
As seen in Table 2, variables such as preparation time, surgical time, estimated blood loss, hospital stay, and decreased hemoglobin level were not different between the two groups. The preparation time of both groups were similar, but the surgical time was significantly longer in the RSS group than in the LESS group. No conversions from minimally invasive surgery to laparotomy or abdominal surgery were required in any of the 109 cases. Additional trocar insertion was necessary in two LESS cases due to severe adhesion from a previous surgical history. There were one and two umbilical hernia cases in the RSS and LESS groups, respectively. All three of these umbilical hernia cases belong to an initial period of single-site surgery in our institution and were of patients who were relatively obese. After excluding the cases of unscheduled emergent surgery, the amount of estimated blood loss was less in the LESS group, but the hemoglobin level showed no difference between the groups. The surgical time was still longer in the RSS group.
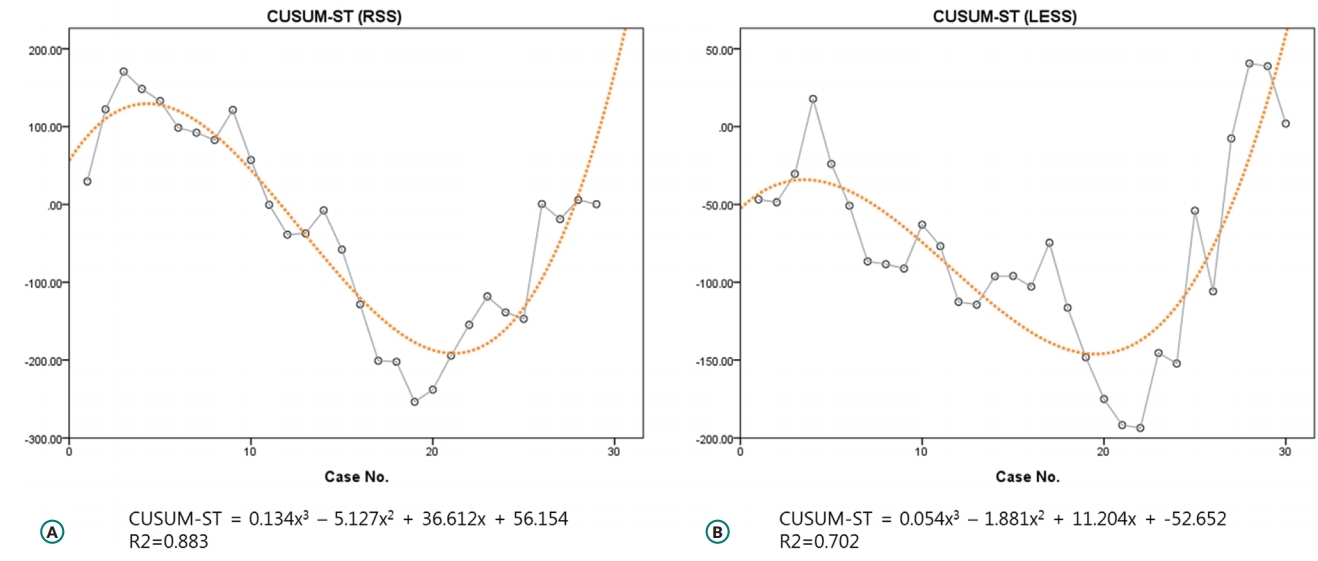
Fig. 2 shows the docking time plotted chronologically according to the case number. This learning curve was obtained by plotting the cumulative sequential differences between each data point and the average docking time, using CUSUM, which was best modeled as a third-order parabola (CUSUM-DT). It showed a main slope change after the 7th case, making an initial positive slope followed by a negative slope. We also compared the learning curves of surgical time for the two groups (CUSUM-ST). In RSS, a triphasic curve was most suitable for CUSUM-ST, which showed a main slope change after 19 cases (Fig. 3A). A similar pattern was observed for the first 30 cases of LESS, but the slope changed after 22 cases (Fig. 3B).

Learning curve for docking time in robotic single-site surgery. CUSUM-DT, cumulative sum of docking time.
DISCUSSION
For the last decades, the introduction of robotics in gynecological operations has been one of the most remarkable advances in the field of minimally invasive gynecologic surgery [7]. In Korea, there is a clear trend of increasing use of robotic systems not only in oncologic surgery, but also in benign surgery [8]. RSS surgery is the most advanced technique in the field of robotic surgery, but its application is limited to selective patients due to the lack of national insurance coverage for robotic surgery in South Korea [9]. In addition, many surgeons feel uncomfortable about using the RSS system compared to the multiport robotic system and complain about the limited range of movement, insufficient strength of the robotic arms, and lack of articulation. However, single-site surgery has its own benefits such as an invisible or less scarring surgical incision, and it is reasonable when compared to LESS surgery rather than multiport robotic surgery [10].
Our data shows comparable surgical outcomes for RSS ovarian cystectomy. In our institution, there is no absolute indication of minimally invasive surgery conducted via either robotic or laparoscopic method. Surgeons decide which patients are suitable for robotic surgery and give them information about robotic surgery. Single-site surgery is usually performed on younger patients who are relatively sensitive about surgical wounds and scarring. In this study, RSS showed similar levels of blood loss, transfusion rates, lengths of stay, and wound complication rates such as hernia. However, RSS surgery had a longer surgical time than LESS surgery. After exclusion of emergency surgeries, the amount of estimated blood loss (EBL) in the operative record was larger in the RSS group. However, the rates of transfusion and hemoglobin levels showed no difference between the two groups. The EBL in the medical record could be inaccurate or omitted in certain circumstances. The surgical time was still longer in RSS surgery than in elective LESS surgery. Paek et al. [11] reported a similar outcome in an analysis of single-site surgeries of adnexal tumors. This is inevitable due to the necessary time for docking the robotic system to the patients. This does not only mean the time for initial docking, but also includes the time for changing robotic instruments, cleaning the camera, undocking, scrubbing, and donning the surgical clothes for the surgeon. Additionally, there is also a risk of error with robotic instruments. It is not surprising that RSS surgery had a longer surgical time considering these aspects.
In an analysis of the learning curve, the docking in RSS surgery did not require many cases to attain sufficient skills. In our study, the surgeon was adept at docking in RSS surgery after only seven cases. This was even faster than CUSUM-DT of multiport robotic surgery in radical hysterectomy previously reported from our institution [12]. The initial docking would be complicated because of the paradoxical positioning of the robotic arms, but once it reaches a proficiency, it is easier to dock because it does not require interport distance or consideration of the diversity of each patient’s abdominal extent [13]. In CUSUM-ST, RSS surgery required fewer cases to attain proficiency than LESS surgery. This is a definite benefit of the robotic system [14] and many surgeons could be familiar with single-site surgery using a robotic system even if they felt somewhat uncomfortable when performing LESS surgery.
This study has several limitations. First, this cohort represents a small window to the learning curve data of a single surgeon, which may not be generalizable to others. However, the single surgeon experience is important to consider, when taking into account that this surgeon has the widest experience of diverse gynecologic surgery in our country. Second, the patient data were obtained retrospectively, and selection bias could impact the results. However, the patient demographics were not different between the two groups, and we also conducted the evaluation excluding emergency surgeries for a more objective comparison.
In conclusion, the surgical outcomes of RSS ovarian cystectomy were comparable to those of LESS ovarian cystectomy. RSS ovarian cystectomy could be performed safely without complications and the RSS system requires fewer cases to gain proficiency in the learning curve of surgical time in initial cases. The long surgical time may be improved by further experience and technical refinements.
Notes
No potential conflict of interest relevant to this article was reported.