Robotic radical hysterectomy for early-stage cervical cancer: A systematic literature review
Article information
Abstract
Robotic technology has recently come into widespread use to overcome the limitations of laparoscopic radical hysterectomy in the treatment of early-stage cervical cancer. Most comparative studies showed that blood loss and hospital stays for patients undergoing minimally invasive surgery, including robotic procedures, were superior compared to open surgery. Moreover, the survival outcomes of robotic radical hysterectomy were not inferior to open radical hysterectomy. Unexpectedly, the Laparoscopic Approach to Cervical Cancer (LACC) trial, a randomized, open-label, noninferiority study that compared minimally invasive radical hysterectomy with open radical hysterectomy, revealed that minimally invasive surgery was associated with a higher risk of recurrence and death compared with open surgery. Strict guidelines for robotic radical hysterectomy for the treatment of early-stage cervical cancer should be established in accordance with objective Korean data. In addition, it is recommended that further studies should be performed on how to avoid the use of uterine manipulators and the dissemination of cancer cells by ensuring a more effective vaginal closure using a standardized approach.
INTRODUCTION
Radical hysterectomy (RH) is a well-established treatment modality of early-stage cervical cancer. RH is defined as the en bloc removal of the uterus and cervix with the surrounding parametrial tissue and upper vagina. Since the introduction of conventional laparoscopy, improvements in gynecologic surgery have been notable. However, laparoscopic RH (LRH) remains a rather unpopular choice among gynecologic oncologists because of the increased operative time and the steep learning curve required for competency [1]. Robotic technology has recently come into widespread use to overcome the limitations of laparoscopic surgery [2]. This is because robotic surgery provides more surgical options, such as nerve-sparing technique, due to its superior visualization (3-dimensional imaging of the operative field), mechanical improvement (seven degrees of instrument mobility inside the body) and stabilization/tremor filtration of the instrument within the surgical field [2].
Unexpectedly, the Laparoscopic Approach to Cervical Cancer (LACC) trial, a randomized, open-label, noninferiority study that compared minimally invasive RH with open RH (ORH), found that minimally invasive surgery (MIS) was associated with a higher risk of recurrence and death compared with open surgery. Female patients randomized to the minimally invasive surgery arm experienced an almost four times greater risk of recurrence and six times greater risk of death compared with female patients that were randomized to laparotomy [3]. In a statement released after the publication of the LACC trial, the Society of Gynecologic Oncology encouraged surgeons to discuss these data with patients undergoing surgery for cervical cancer [4], and the National Comprehensive Cancer Network cervical cancer guidelines were revised accordingly to define the open abdominal approach as the “standard and recommended approach to RH” [5].
Consequently, this study performed a systemic literature review to appraise and synthesize the available real-world evidence on robotic RH (RRH). Moreover, we compared the risk of recurrence and death between patients who underwent MIS vs. ORH for early-stage cervical cancer.
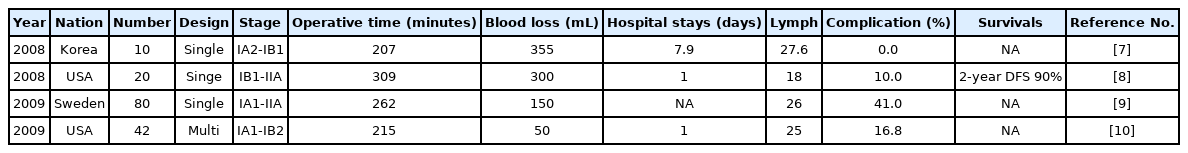
CASE SERIES OF RRH
After Marchal et al. [6] performed RRH in 2005, several case series of RRH were published (Table 1) [7-10]. In Korea, Kim et al. [7] for the first time reported 10 cases of RRH and concluded that RRH for selected patients with IB1 cervical cancer is feasible, promising and related with a low morbidity (Table 1).
MIS (ROBOT AND LAPAROSCOPY) VS. OPEN
Most initial comparative studies between MIS and ORH focused on the respective surgical outcomes [11-14]. Most comparative studies showed that blood loss and hospital stays for the MIS group were superior compared to the open group [11-17]. Furthermore, previous retrospective comparative studies revealed that the survival outcomes of MIS were comparable to the survival outcomes of open surgery [15-17]. In the LACC trial, however, MIS was associated with a lower range of disease-free survival (DFS; 3-year rate, 91.2% vs. 97.1%; hazard ration [HR], 3.74; 95% confidence interval [CI], 1.63–8.58) and overall survival (OS; 3-year rate, 93.8% vs. 99.0%; HR, 6.00; 95% CI, 1.77–20.30) [3]. Following the LACC trial, several retrospective comparative studies reported on the survival outcomes of MIS and open surgery [18-20]. Cusimano et al. [18] showed that MIS was associated with increased rates of death (HR, 2.20; 95% CI, 1.15–4.19) and recurrence (HR, 1.97; 95% CI, 1.10–3.50) after adjusting for individual patients’ factors and surgeon volume. Moreover, an international European cohort observation study (the SUCCOR study) demonstrated that the risk of recurrence for patients who underwent MIS was twice as high compared to the open surgery group (HR, 2.07; 95% CI, 1.35–3.15; P=0.001). Similarly, the risk of death was 2.42-times higher than in the open surgery group (HR, 2.45; 95% CI, 1.30–4.60, P=0.005) [19]. Finally, Brandt et al. [20] reported that MIS RH did not confer worse oncologic outcomes in a singlecenter retrospective study (Table 2).
ROBOT VS. OPEN SURGERY
Most comparative studies showed that blood loss and hospital stays for the robot group were superior to those of the open group [21-31]. However, the majority of these studies demonstrated that the operative time of ORH was significantly shorter compared to RRH [21,23,26,28,29]. The survival outcomes of RRH and ORH were first reported in 2010, and for a 3-year progression free survival (PFS) were 94% in RRH and 89% in ORH (P=0.27) and the 3-year OS were 94% in RRH and 93% in ORH (P=0.47), respectively [24]. After this study [24], several retrospective comparative studies showed that survival outcomes were similar between the two groups [28,29,31]. However, Wallin et al. [30] used a multivariate regression analysis and demonstrated that RRH was significantly more associated with tumor recurrence (HR, 2.13; 95% CI, 1.06–4.26; P<0.05). Moreover, abdominal radical hysterectomy had a greater PFS advantage over RRH for tumors ≥2 cm (HR, 0.31; 95% CI, 0.11–0.90; P=0.04) [32]. Furthermore, recent retrospective studies have also reported poor survival outcomes in RRH compared to ORH after propensity score matching (Table 3) [33,34].
ROBOT VS. LAPAROSCOPY
Surgical outcomes, such as the operative time and comlication rate were different for different studies [35-45]. However, most studies reported that blood loss of RRH was superior to that of LRH [35,37-39,45]. Finally, several retrospective studies have reported similar survival outcomes between the two groups (Table 4) [36-38,41,42,44,45].
ROBOTIC SINGLE-SITE RH
Sinno and Tanner [46] reported the first surgical film of robotic single-site RH. Recently, Jang et al. [47] compared the surgical outcomes of robotic single-site and multiport RH. Hospital stay and total hospital cost for single-site were significantly shorter and lower, respectively, compared to multiport surgery (P<0.01) [47].
NATIONWIDE POPULATION-BASED STUDIES
In an epidemiologic study performed in the USA, MIS was associated with shorter OS rates compared to open surgery (HR, 1.65; 95% CI, 1.22–2.22; P=0.002) [48]. In contrast, nationwide population-based studies in Scandinavia, reported different outcomes [49,50]. For instance, a Swedish nationwide population-based cohort study showed that the 5-year OS was 94% and 92%, and DFS was 88% and 84% for the robotic and open cohorts, respectively [49]. Moreover, the 5-year OS after propensity score matching was 92% for both cohorts (HR, 1.003; 95% CI, 0.5–2.01; P=0.99) [49]. In a Danish nationwide population- based cohort study, adoption of RRH for early-stage cervical cancer was not associated with either an increased risk of recurrence or reduction in survival outcomes [50].
ISSUES OF TUMOR SPILLAGE IN MIS
In the LACC trials, the potential reasons for the inferior oncologic outcomes in the MIS included the routine use of uterine manipulator, effect of the insufflation gas (CO2) on tumor-cell growth and that spread might increase the propensity for tumor spillage [3]. In the SUCCOR study, the use of uterine manipulator during MIS was associated with worse 4.5-year DFS (82% vs. 93%; HR, 3.48; 95% CI, 1.17–9.48, P=0.028) and 4.5-year OS (88% vs. 96%; P=0.016) [19]. Klapdor et al. [51] evaluated peritoneal contamination with indocyanine green stained cervical secretion as surrogate for potential cervical cancer cell dissemination during colpotomy. Peritoneal contamination was detected in 75% (9/12) patients during laparoscopic hysterectomy and uterine manipulator contamination was detected in 60% [51]. However, Nica et al. [52], reported that the use of intrauterine manipulator in patients with early cervical cancer who underwent MIS was not an independent factor with a significant rate of recurrence after controlling for adverse pathological factors (HR, 0.4; 95% CI, 0.2–1.0; P=0.05). Kong et al. [53] demonstrated that the rate of disease recurrence was higher in the intracorporeal colpotomy group compared to the vaginal colpotomy group (16% vs. 5%), and among patients with recurrence in the intracorporeal group, 62% had intraperitoneal spread or carcinomatosis. The author concluded that exposure of cervical cancer to circulating CO2 may result in tumor spillage into the peritoneal cavity [53]. Furthermore, other previous studies also presented intraperitoneal recurrences only in robot or MIS during RH [33,42].
UPCOMING TRIALS
Two novel noninferiority randomized controlled trials (RCTs) have been launched in terms of evaluating early-stage cervical cancer following the publication of the LACC trial results. The first one is a multicenter Chinese trial that compares RRH or LRH vs. ORH with DFS at 5 years as its primary objective, which has a planned sample size of 1,488 patients from 28 participating centers with an individual surgeon case volume [54]. The second one is performed in an international multicenter RCT (Robot-assisted Approach to Cervical Cancer [RACC] trial), and compares RRH vs. ORH with the 5-year DFS as its primary end-point and a planned sample size of 800 patients [55].
CONCLUSION
The authors of the LACC study and the US Cancer Resist Evaluation stated that MIS RH was associated with a higher rate of recurrence and poorer OS compared to ORH. Previous meta-analysis based on retrospective studies, showed that open surgery had no significant superiority.
The results were not interpreted as the end of MIS in terms of treating cervical cancer; instead, it was recommended that studies should be performed on how to avoid the use of uterine manipulators and the dissemination of cancer cells by ensuring a more effective vaginal closure using a standardized approach.
In agreement with previous nationwide population-based studies, our findings underline a disagreement on survival outcomes according to the specific conditions and parameters of each nation. Therefore, it is necessary to perform a Korean nationwide population-based study that will focus on the respective oncologic outcomes. Furthermore, strict guidelines for MIS in the treatment of early-stage cervical cancer should be implemented which will be consistent with objective data from the Korean population.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.